PCOS – A Common but Often Hidden Hormonal Imbalance
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders affecting women – yet many live with it without even realising. Symptoms may begin during the teenage years with irregular periods or acne, or not appear until later in life when hormonal shifts occur during menopause.
It’s estimated that 10–15% of women live with PCOS, but for many, the diagnosis remains hidden. So what exactly is this syndrome, why does it affect so many, and what does current research say about future treatments?
WHEN DOES IT START – AND HOW LONG DOES IT LAST?
Symptoms of PCOS often appear in adolescence, but a diagnosis requires meeting specific medical criteria.
Many experience their first symptoms as teenagers. Periods may be delayed, highly irregular, or absent for long stretches. Skin and hair changes may also occur, such as persistent acne or increased hair growth compared to peers.
Despite this, many aren’t diagnosed until their 20s or 30s – often when seeking help for fertility issues.
PCOS is a chronic condition that can change over time. While some symptoms may ease after menopause, the hormonal imbalance can continue to affect metabolism, weight, and the risk of related conditions like type 2 diabetes and cardiovascular disease.
HOW PCOS IS DIAGNOSED
Diagnosis is based on the internationally recognised Rotterdam criteria, which require at least two of the following three to be present:
Irregular or absent ovulation/periods – cycles are infrequent, highly irregular, or absent for extended periods.
Signs of elevated male hormones (androgens) – such as acne, increased hair growth on the chin, abdomen or chest, or thinning hair on the scalp. These hormone imbalances may also be detected through blood tests showing higher-than-normal testosterone levels.
Polycystic ovaries on ultrasound – multiple small, undeveloped follicles appear in the ovaries. These do not mature and release eggs as they should, resulting in irregular or absent ovulation. It’s important to note that these cysts are not dangerous and should not be confused with pathological ovarian cysts.
CAN YOU HAVE PCOS WITHOUT KNOWING IT?
Yes – many women never receive a formal diagnosis. If menstrual irregularities during adolescence gradually resolved, PCOS may go unnoticed. Some only become aware of the condition when trying to conceive, while others may never undergo investigation at all.
For some, symptoms of PCOS become more pronounced during the menopause. As oestrogen levels decline, the hormonal imbalance becomes more noticeable, potentially increasing issues such as weight gain, blood sugar instability, or dryness and thinning of the vaginal tissues.
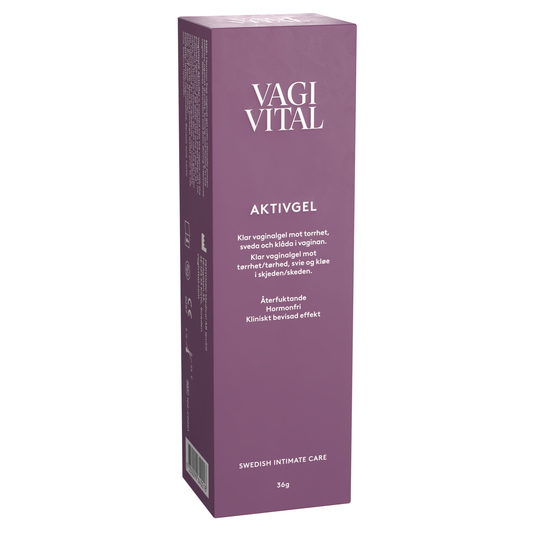
🌸 VagiVital AktivGel is a clinically proven, hormone-free treatment that deeply hydrates and rebuilds the vaginal mucosa. It is designed for long-lasting effect and can make a real difference for those experiencing dryness and discomfort linked to PCOS or menopause.
👉 Buy VagiVital AktivGel here
WHAT CAUSES PCOS?
The exact cause of PCOS isn’t fully understood, but research suggests both genetic and metabolic factors are involved.
🌸 Genetics – Twin studies show a strong hereditary component. If your mother or sister has PCOS, your own risk is increased.
🌸 Insulin resistance – The body may respond abnormally to insulin, the hormone that regulates blood sugar. This can lead to elevated insulin levels, which in turn stimulate the ovaries to produce more testosterone. This disrupts hormonal balance and ovulation.
🌸 Inflammation – Several studies suggest a connection between PCOS and low-grade, chronic inflammation. This is not a localised infection but a general, subtle immune response that can affect hormones and metabolism over time.
HOW DO YOU KNOW IF YOU HAVE PCOS?
Since many symptoms – such as irregular periods, acne, weight gain or fatigue – can also occur without PCOS, a full medical assessment is always required.
A typical investigation includes:
🌸 Medical history and symptom discussion – including menstrual patterns and any related issues
🌸 Blood tests – to assess hormone levels, blood sugar, and lipid profiles
🌸 Ultrasound scan – to check for polycystic ovaries
💜 Important: Not everyone with ovarian cysts has PCOS. Ultrasound findings must be interpreted in combination with hormone levels and clinical symptoms.
WHO TO CONTACT FOR HELP
The first step is to contact your GP or a gynaecologist. If you suspect PCOS, you can request an investigation. If fertility is a concern, you may be referred to a fertility clinic or an endocrinologist (a hormone specialist).
In larger cities, specialist clinics with expertise in PCOS are available. Support groups and patient communities can also be a valuable resource – especially for sharing experiences and feeling seen ❤
TREATMENT AND SOLUTIONS GOING FORWARD
There is currently no cure for PCOS, but many ways exist to manage symptoms and reduce the risk of related conditions. Treatment is always tailored to your stage of life and the symptoms affecting you most.
Lifestyle as the Foundation
For many, the first step is to support the body through everyday habits: regular physical activity, good sleep, stress management and blood sugar–friendly nutrition. Even modest, sustainable weight loss in cases of overweight can improve hormonal balance and support ovulation.
Cycle Regulation and Skin/Hair – When Pregnancy Is Not the Goal
Some choose hormonal contraceptives (e.g. the pill, vaginal ring, or hormonal coil) to make bleeding more regular and to ease symptoms such as acne or excess hair growth. These can improve quality of life but are not a “cure” for PCOS. The choice of treatment should always be made with a doctor, weighing benefits and risks.
Protecting the Uterine Lining When Periods Are Infrequent
If periods are very infrequent, doctors may suggest treatments to protect the uterine lining. This may involve taking progestogens (a hormone similar to the body’s own progesterone) in short courses a few times a year, or using a hormonal IUD that releases small amounts of hormone locally. Both options work by keeping the uterine lining thin and reducing the risk of cellular changes.
Medications That Affect Insulin
In some women with PCOS, insulin resistance plays a major role. This can make it harder to regulate blood sugar and contributes to hormonal disruption. In such cases, doctors may prescribe medications commonly used for diabetes. Studies show these can improve blood sugar control, weight, and hormone levels in some women – though they are not suitable for everyone and require monitoring. Newer medications that affect both appetite and blood sugar are currently being studied as potential treatments for PCOS.
WHEN YOU WANT TO HAVE CHILDREN
When pregnancy is the goal, the treatment approach shifts. The focus becomes stimulating ovulation, rather than just regulating the cycle. This is done through medication and always in consultation with a gynaecologist or fertility clinic. Many women with PCOS do become pregnant – sometimes spontaneously, sometimes with medical support.
FUTURE TREATMENTS
PCOS research has long been underfunded, but interest is growing. Scientists are increasingly exploring connections between gut health, inflammation and new treatment options. For example, researchers are investigating whether probiotics or GLP-1 analogues (drugs currently used for diabetes and obesity) could also benefit women with PCOS.
🌱 Want to learn more about the link between gut health and vaginal wellbeing?
👉 Read our blog “Gut Health and Vaginal Health – What’s the Connection?” here https://vagivital.uk/blogs/news/gut-health-and-vaginal-health-whats-the-connection
INTIMATE HEALTH AND PCOS
Hormones affect the entire body – including the vagina and vulva. Women with PCOS may experience periods of dryness or sensitivity, particularly when periods are absent or hormone levels fluctuate. This can lead to irritation, discomfort, or pain during sex.
One safe way to support your body is by caring for your intimate health with the Stay Pussytive Kit – a complete set of four products designed to hydrate, cleanse, and soothe both the vagina and vulva:
💜 AktivGel – clinically proven, hormone-free treatment for vaginal dryness
💜 Active Glide – moisturising lubricant developed especially for women ❤
💜 V Cleanser – gentle, soap-free intimate wash
💜 Calming Gel – soothes irritation and vulval sensitivity
👉 Learn more and buy the Stay Pussytive Kit with 10% off here
LIVING WITH PCOS
Receiving a PCOS diagnosis can raise concerns – especially around fertility. But it’s important to know that many women with PCOS do become pregnant, either naturally or with medical support.
PCOS is one of the most researched gynaecological conditions. Thousands of scientific articles are published each year, covering everything from genetics, fertility, hormones and metabolism to mental health. This means knowledge is continually growing, and healthcare providers are gaining more tools to support women.
With the right care, support and information, it is absolutely possible to live well with PCOS – while taking care of both your present and your future health ❤
Take care of yourself & Stay Pussytive ❤
Fanny Falkman Grinndal Business Manager Nordics Peptonic Medical AB fanny.falkman-grinndal@peptonicmedical.se
SOURCES
• Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004. • Teede HJ, et al. International evidence-based guideline for the assessment and management of polycystic ovary syndrome 2018. Hum Reprod. 2018. • Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocr Rev. 1997. • Glintborg D, et al. Endocrine and metabolic characteristics in polycystic ovary syndrome. Nat Rev Endocrinol. 2023. • Torres PJ, et al. Gut microbiome in women with polycystic ovary syndrome: a systematic review. Reprod Sci. 2018. • Elkind-Hirsch KE, et al. Efficacy of GLP-1 receptor agonist therapy in women with polycystic ovary syndrome: A randomised trial. J Clin Endocrinol Metab. 2022.
Recommended products for you
- Choosing a selection results in a full page refresh.
- Opens in a new window.