That is why you can get a yeast infection in the vagina from antibiotics
Why do vaginal problems always occur around long weekends? That was exactly the case last Christmas. Surrounded by the scent of freshly baked saffron buns, burnt toffee, and endless Christmas music playing from the speakers, I struggled with a stubborn sinus infection. After trying to let it heal on its own, without success, I finally gave up and had to surrender to a course of antibiotics. I have had several yeast infections in my life, and antibiotics have always been the culprit. But this time I had either forgotten, repressed it, or was perhaps just too busy thinking about Christmas Eve approaching and the sinus infection being super annoying combined with all the preparations for Christmas. It had been years since I last experienced a vaginal yeast infection and I naively hoped I would escape this time. But of course, I was completely wrong. On the third day of antibiotic treatment, that familiar, itchy feeling started to make itself known. Slightly itchy tingling in the vulva signaled that something was wrong. "Not now, please," I thought. But yes, just like an uninvited guest, the yeast infection appeared when I least wanted it. It's almost as if vaginal problems have a built-in calendar and deliberately choose the absolute worst possible times, such as weekends and public holidays, when access to a gynecologist is as limited as Santa Claus on Christmas Day. That is why it will be especially exciting that VagiVital in 2024 will launch many clinically proven products that can diagnose, treat, and prevent genital problems, such as yeast infections❤.
THIS IS WHAT HAPPENS IN THE VAGINA WHEN YOU TAKE ANTIBIOTICS
Antibiotics are effective medicines for fighting bacterial infections, but their action is not selective. This means that when you take antibiotics to fight a specific harmful bacterium, the beneficial bacterial flora in the body, including in the vagina, is also affected. The vagina is naturally home to various types of bacteria and microorganisms, where the good bacteria, such as lactobacilli, play a central role.
Lactobacilli are especially important because they help maintain an acidic pH in the vagina, which is crucial for a healthy vaginal environment. The acidic pH prevents the overgrowth of harmful organisms, including fungi like Candida. These fungi naturally exist in small amounts in the vagina but are kept in check by the acidic environment and the competition posed by the good bacteria.
When antibiotics remove these protective lactobacilli, the vaginal pH balance is disturbed. This can lead to increased alkalinity, meaning the pH value rises, creating a favorable environment for fungal growth. As a result, fungi such as Candida albicans, which normally exist in the vagina without causing problems, begin to grow uncontrollably. This leads to yeast infections in the vagina, characterized by symptoms such as itching, irritation, and sometimes a thick, white discharge.
In the vagina, lactobacilli, a type of good bacteria, play a key role. They produce lactic acid that helps keep the vaginal environment acidic, which is important to limit the growth of Candida albicans and other potentially harmful microorganisms. This acidic environment is crucial for vaginal health and helps prevent infections.
Read the blog on how to keep the vaginal flora healthy here!
WHEN THE FUNGUS CANDIDA ALBICANS TAKES OVER
Candida albicans is a type of yeast fungus that naturally occurs in the human body, including in the mouth, intestines, and vagina. In a healthy body, the presence of Candida albicans is usually insignificant and causes no problems. This is because it is kept in check by the body's natural microflora – a balanced collection of microorganisms, including bacteria, that help maintain a healthy environment.
Problems begin when the balance of the vaginal microflora is disturbed, which can happen for various reasons, such as antibiotic use, hormonal changes, weakened immune system, high stress levels, or dietary changes. When the balance is disrupted, it can lead to uncontrolled growth of Candida albicans, resulting in a yeast infection known as vaginal candidiasis or a yeast infection in the genital area.
Candida albicans, although best known for causing infections when it grows uncontrollably, actually also has certain roles in the body under normal circumstances:
🌺 Part of the normal microflora
Candida albicans naturally exists in the body, especially in the intestines, on the skin, and in genital areas. Under normal, healthy conditions, it is part of the body's microflora – the collection of microorganisms living in and on the body. These organisms, including Candida, contribute to some extent to the body's ecosystem and its functions.
🌺 Contributes to microbial balance
In a healthy individual, Candida albicans helps maintain a balance with other microorganisms. When this balance is intact, different microbes, including Candida, compete with each other, preventing any single organism from becoming too dominant.
🌺 Potential role in the immune system
Candida albicans may also play a role in the immune system. The presence of these microorganisms, including Candida, helps "train" the immune system so that it can respond more effectively to pathogenic microorganisms. This interaction may contribute to a better ability to distinguish between harmful pathogens and harmless or even beneficial microorganisms.
🌺 Possible impact on digestion
Although this role is not as clearly defined for Candida albicans as for some other gut microbes, it and other yeasts may contribute to certain aspects of digestion and nutrient absorption.
It is important to remember that problems with Candida albicans arise when its growth becomes uncontrolled, which can lead to infections such as yeast in the genital area. The threshold for when Candida albicans becomes "troublesome" is when symptoms become noticeable and cause discomfort or pain.
SYMPTOMS OF CANDIDA INFECTION
Symptoms of vaginal yeast infection include itching, redness, irritation in the vagina and vulva, pain during intercourse, and a thick, white discharge often compared to cottage cheese. These symptoms occur when the growth of Candida albicans becomes extensive enough to cause irritation and inflammation in the vaginal tissues.
Read the blog on how to get rid of yeast infection in the genital area here!
CHOOSE ANTIBIOTIC-FREE TREATMENT FOR BACTERIAL VAGINOSIS
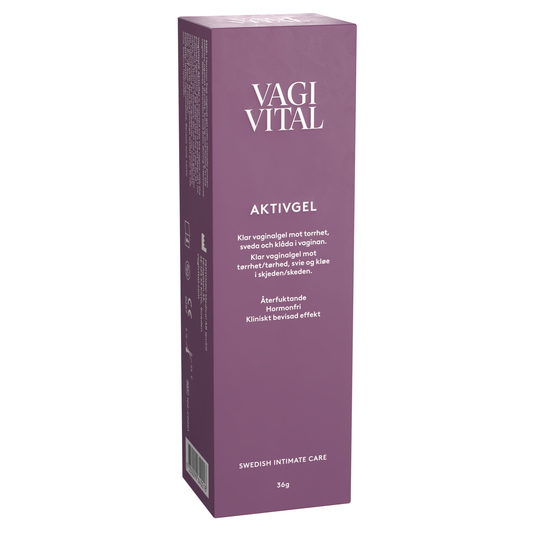
To prevent overgrowth of Candida albicans and maintain a healthy vaginal flora, it is important to avoid unnecessary use of antibiotics and use mild, fragrance-free intimate products. VagiVital V Cleanser is a gentle and moisturizing intimate wash that cleanses without disturbing the vaginal microflora or pH.
You can find VagiVital V Cleanser here!
Yeast infections that occur after antibiotic treatment are usually not serious, but they can cause discomfort and trouble. Additionally, recurring yeast infections may be a sign of disturbed vaginal flora, which may require further treatment or lifestyle changes to restore the natural balance.
Women with bacterial vaginosis, a common vaginal imbalance, are often prescribed antibiotics. Although this may seem like an effective solution, paradoxically it can contribute to further imbalance by disturbing the natural flora in the vagina.
Read the blog about foul-smelling discharge caused by bacterial vaginosis here!
Here comes Vernivia vaginal mousse into the picture ❤. Vernivia is an antibiotic-free treatment specially designed to treat foul-smelling discharge caused by bacterial vaginosis. Unlike traditional antibiotics, Vernivia supports the natural flora in the vagina as it restores pH balance and works by mimicking the vagina's own immune defense where the growth of the good lactobacilli is stimulated. By choosing Vernivia, you avoid the negative side effects that often accompany antibiotic treatment, such as the risk of yeast infections. This makes Vernivia an ideal choice for women seeking a gentle, effective, and balancing solution to the problem of bacterial vaginosis. The effect is clinically proven and equivalent to prescription antibiotics❤
The over-the-counter antifungal medications available on the market today have unfortunately never worked for me, but luckily I had a fantastic general practitioner who could step in and save the situation. Thanks to this, I was yeast-free just in time for the Christmas celebrations. But the experience has taught me that antibiotics and yeast infections for me are as certain as Christmas coming every year. Next time I face the choice of taking antibiotics, I will think twice or even thrice. Unless it’s my Christmas preparations, that is 😊
Take care & Stay Pussytive ❤
/Fanny
Recommended products for you
- Choosing a selection results in a full page refresh.
- Opens in a new window.