This is how you get rid of a yeast infection in the genital area
Are your mucous membranes as dry as a desert with a blazing redness that itches and stings? Maybe you also have a cottage cheese-like, whitish discharge?
Yes, then you have probably got a yeast infection!
HOW COMMON ARE YEAST INFECTIONS IN THE GENITAL AREA
You are not alone with this condition! About 75% of all women suffer from a yeast infection in the genital area at some point in their lives, and everyone who has ever had it knows that it can be extremely distressing! Fortunately, most yeast infections are easily treated with local or oral antifungal agents, and after that, the symptoms usually disappear, but some, mostly aged 25–34 years, have a higher risk of recurrent yeast infections.
RECURRENT YEAST INFECTIONS
So what counts as recurrent yeast infection? Well, it is usually said that you should have at least 3–4 yeast infections per year for it to be defined as recurrent vulvovaginal candidiasis (RVVC), i.e., recurrent chronic yeast infections, which affect about 6-9% of women of reproductive age.
This can be extremely troublesome and often requires regular contact with healthcare, as RVVC can be difficult to treat.
PAIN DURING INTERCOURSE
An undertreated yeast infection can lead to pain during intercourse. Many women with pain in the genital area, so-called vulvar pain (vestibulodynia), also report having had repeated yeast infections previously. Vulvar pain means that it can also be difficult to use tampons, wear tight clothes, cycle, and ride.
CAUSE OF CHRONIC YEAST INFECTION
There are several factors that can contribute to a woman developing chronic yeast infection (RVVC), and it can also be a combination of several different risk factors. Some of the most common are:
- Ongoing or recently completed antibiotic treatment,
- Diabetes
- Pregnancy
- Cytostatic treatment
- Hormonal factors
- In chronic yeast infection (RVVC), it is also common to have an additional vaginal condition such as bacterial vaginosis or vulvar pain (vulvodynia).
HOW TO SUCCESSFULLY TREAT YEAST INFECTIONS IN THE GENITAL AREA
Single yeast infections in the genital area are often successfully treated with over-the-counter medications or a single dose of antifungal agents prescribed by a doctor. However, living with recurrent vaginal yeast infections can affect both quality of life and intimate relationships, but there is light at the end of the tunnel!
The first step with recurrent yeast infections is to seek help from a gynecologist/youth clinic and perform a yeast culture to find the right treatment. When doing a culture, it is also important that you have ongoing symptoms at the time of sampling and that you have not used any antifungal agents in the last 2–3 weeks.
Unfortunately, there is still no 100% curative treatment for chronic yeast infection, but long-term treatment with prescription antifungal agents combined with emollient and moisturizing treatment is successful in many cases.
CLEAN WITHOUT SOAP
Cleaning the intimate area with soap risks drying out the sensitive mucous membranes and disturbing the pH balance, which can also worsen the yeast infection.
Our patented gentle and caring VagiVital V Cleanser is an intimate wash that is both different and completely unique on the market!
This product has the same moisturizing and unique properties as VagiVital AktivGel but with some added rapeseed oil. Soap risks drying out the vagina. Oil can bluntly only remove fat-soluble impurities. This is where VagiVital V Cleanser comes in! Although it is soap-free, it can clean both fat- and water-soluble impurities while moisturizing without disturbing the genital area's sensitive pH balance. This reduces itching, treats dryness, and prevents cracking, which worsens the yeast infection.
You can find VagiVital V Cleanser here
A HAPPY VAGINA IS A MOIST VAGINA ❤
Dry mucous membranes sometimes give the same symptoms as a yeast infection with burning, itching, and irritation, and small cracks can occur that also make it easier for the yeast to take hold. The vaginal mucosa needs moisture to feel good, and with dry mucous membranes, the bacterial flora is often affected, which increases the risk of yeast infection. A happy vagina is a moist vagina ❤
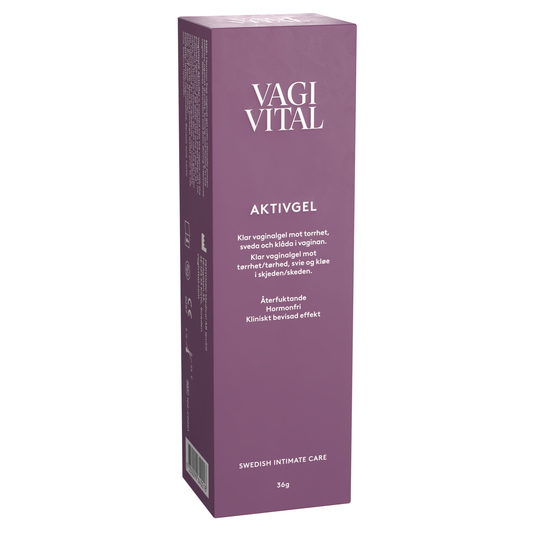
VagiVital AktivGel is a hormone-free active gel that moisturizes the driest mucous membranes, reduces itching, and prevents cracking, which in turn reduces the risk of yeast infection.
You can find VagiVital AktivGel here
FUTURE RESEARCH
There is a need to develop new treatments for yeast infections, and studies are ongoing to find new, effective treatment methods. There are also studies investigating a new vaccine that could reduce recurrences in women with chronic recurrent yeast infections. They have also tested whether the administration of lactobacilli vaginally or orally can work as a preventive treatment against vaginal yeast, but currently, there is no scientific evidence supporting probiotic treatment – there are no sufficiently good studies that have been able to evaluate this.
Yeast infections are today often treated with so-called antimycotic drugs. Since the yeast infection often recurs, women are often treated repeatedly, which has caused the yeast to develop resistance to the drug. Therefore, a drug is needed that can both prevent the problems from recurring and at the same time does not contain antimycotics.
IT IS IMPORTANT TO MAKE A DIAGNOSIS
It can sometimes also be difficult to distinguish between yeast infection and bacterial vaginosis, as the symptoms often can resemble each other. Read more about bacterial vaginosis here!
Since many women are not aware of bacterial vaginosis, they often treat themselves for yeast infection (as the symptoms resemble each other), which causes the symptoms to persist. In 10–15 percent of cases, bacterial vaginosis and candida (yeast infection) occur simultaneously, which requires two different treatments.
VagiVital VS for vaginal infections is a self-test that you can calmly do at home. In 30 seconds and with 92% accuracy, you get an answer as to whether you have a vaginal infection.
You can find VagiVital VS for vaginal infections here
Recommended products for you
- Choosing a selection results in a full page refresh.
- Opens in a new window.